How To Repair A Fracture
Breaks in the pelvis or acetabulum of the hip articulation are amidst the most serious injuries treated by orthopedic surgeons. Oftentimes the issue of a traumatic incident such as a motor vehicle accident or a bad fall, pelvic and acetabular fractures require rapid and precise treatment and, in some cases, one or more than surgical procedures. People of all ages are vulnerable to these injuries. In add-on, some elderly patients with fragile basic due to osteoporosis develop pelvic fractures and fractures of the acetabulum with a lower impact fall.
- Overview of fractured pelvis
- Handling goals
- Nonsurgical treatment
- Surgical treatment
- What are the complications of surgery for a broken pelvis?
- The Orthopedic Trauma Service at HSS
- Frequently asked questions and answers
Overview of a fractured pelvis
The complex nature of these fractures tin can exist better understood by looking at the anatomy that is involved. The pelvis is made upward of several bones (ileum, ischium and pubic basic) which create a bony ring, meeting at the pubic symphysis in the front and the sacrum (a bone situated at the lower stop of the spine) in the back. Together with a number of ligaments and muscles, the bones of the pelvis back up the weight of the upper trunk and rest on the hip joints. The pelvis protects abdominal organs including the intestines and the float, as well as major nerves and claret vessels. Pelvic fractures may occur at any location on the bones depending on the nature of the accident and the areas of bear on.

Radiograph of a normal pelvis

Radiograph of the pelvis demonstrating a fracture of the pubic bone
The acetabulum refers to the part of the pelvis that meets the upper finish of the thigh bone (the femoral head to form the hip articulation. In a healthy hip, these ii bones fit together like a ball and loving cup, in which the ball rotates freely in the loving cup. Cartilage lines the basic where they meet at the joint and there is little friction betwixt the surfaces during movement.
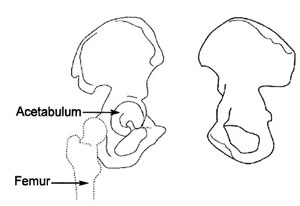
Anatomical illustration of the acetabulum
Most people employ the term "cleaved hip" to refer to a fracture of the brawl side of the joint, that is, a pause in ane of two sections of the femur:
- femoral caput (the "ball" at the very tip of the upper femur)
- femoral neck (a broad department of the upper femur only beneath the femoral head)
In this department, we are speaking specifically of a fracture of the cup or acetabulum. Fractures of the acetabulum are harder to care for because access to this bone is more than difficult, and because of the acetabulum's proximity to the major claret vessels to the legs, the sciatic nervus (the major nerve that arises from the lower spine and provides sensation and move to the leg and human foot), the intestines, the ureter and the bladder. Unlike a hip fracture, which tin can exist treated relatively easily, to repair an acetabular fracture, the orthopedic surgeon, must, in essence, set up the broken bones from the within out.
In fractures of this type, the femoral head is often driven through the acetabulum because of the impact of the fall or accident. If the femoral head ends up outside the acetabulum, this is known as a dislocation of the hip joint. Some patients have both a fracture and a dislocation.

Radiograph of the left hip demonstrating a posterior dislocation of the hip with an associated
Posterior Wall blazon fracture of the acetabulum
Unfortunately, patients with fractures of the pelvis and/or acetabulum, virtually always also experience serious injury to surrounding soft tissue (skin and muscles) and neurovascular structures (nerves, arteries and veins). In addition, particularly in the case of pelvic fractures, adjacent organs can exist seriously injured. With both types of fracture, in that location is pregnant haemorrhage and adventure of nerve damage.
In patients with multiple injuries, treatment begins with the trauma team at the scene, and and then afterwards in the emergency room – a team of full general surgeons, anesthesiologists and nurses – who work together to command bleeding, address harm to the head and breast, and other organs that may have been affected, such equally the bladder and intestines, and to stabilize broken bones. During this early resuscitation phase of treatment, the orthopedic surgeon may need to stabilize the fracture past using an external frame to temporarily hold the basic in proper alignment while other problems are treated. This is called temporary external fixation. Surgeons construct these frames using steel pins that are inserted into the bone and joined together by clamps and rods and tin can do and so very speedily.

Radiograph of the pelvis demonstrating application of a pelvic external fixator.
Once the patient is stabilized – bleeding has stopped and other life-threatening injuries have been addressed – the fractures can be treated definitively. Successful treatment for both of these types of fractures requires the skills of an interdisciplinary team, with orthopedic surgeons working closely with the trauma team (general surgeons), the anesthesiologists and nurses. Post-obit surgery, rehabilitation specialists play a central office in recovery.
Because of the complex nature of these fractures and because many orthopedic surgeons practice not regularly care for them, patients who initially get to a community hospital for emergency attention are ofttimes transferred to an establishment that specializes in such injuries.
Treatment goals
As with any fracture, the main goal of treatment for fractures of the acetabulum and pelvis is to render the patient to their pre-injury functional level, to the greatest extent possible. This ways returning comfortably to daily activities – work and play. Physicians, nurses and rehabilitation specialists design a class of treatment that seeks to get the patient back to total force and with the range of motion that they had before the injury.
To attain these goals, proper alignment of the bones during healing is vital. Patients with acetabular and pelvic fractures often take deportation. In other words, the bones are not in proper position and must be realigned, or put back into identify. Physicians use the term reduction to describe this process.
If a articulation surface malheals (that is, with irregularities), the cartilage that lines the joint will rub together and wear downwardly, setting the phase for astringent arthritis of the articulation, loss of motion, decreased function and hurting.
Nonsurgical treatments
Treatment for patients with pelvic fractures is based on a number of factors including the type of fracture, the stability of the pelvis, and the degree of displacement of the basic. The orthopedic surgeon uses information gathered through physical examination, conventional radiographs and CT scans to make this conclusion. Patients with a stable pelvic fracture – without displacement or dislocation--are the most likely candidates for nonsurgical handling. Some may crave closed reduction (realignment without an open surgical procedure) nether anesthesia with or without external fixation.
Some patients with fractures of the acetabulum itself may also be treated nonsurgically. Usually, this treatment is selected for patients who practice not take displacement and/or those who may not be able to tolerate surgery, such equally individuals with significant medical problems, infections or severe osteoporosis. Closed reduction is washed either through manipulation conducted while the patient is under anesthesia or past putting the patient in traction.
Surgical treatment
Realignment of the bones may be done either as an open reduction, in which the orthopedic surgeon makes an incision to directly manipulate the bone, or as a closed reduction, in which this incision is not necessary. One time the bones are realigned, the surgeon uses internal or external fixation to hold the bone in proper position during healing. Metallic devices including wires, pins, screws, and plates are used.

Radiograph of the pelvis post-obit open reduction and internal fixation (ORIF) of a complex comminuted
fracture of the left acetabulum, hemipelvis and pubic symphysis.
Patients with pelvic fractures may crave one or more surgical procedures. The surgeon may begin with an External Fixation (Ex-Ready) technique in which an open or closed reduction is performed and the bones are and then held in place using an external fixator, or frame. This is done by threading pins into the bone on either side of the fracture. These pins are then connected to rods outside the peel, which form a frame.
While the Ex-Fix technique is sometimes the just procedure needed to repair a fractured pelvis, some patients crave additional surgery or surgeries in which plates and screws are used internally to hold the bones in place. Depending on the site and complication of the fracture, the surgeon may accept to fix the front of the pelvis, the back of the pelvis, or both. Separate operations may exist needed for each area that needs treatment.
Patients with acetabular fractures frequently require an Open Reduction with Internal Fixation (ORIF), especially those patients who besides have displacement of the joint. The surgeon realigns or reduces the bones every bit precisely equally possible to preclude the evolution of post-injury related problems, particularly arthritis. The bones are rigidly fixed with plates and screws to foreclose future displacement and permit for rehabilitation to begin as rapidly as possible.
Fractures of the acetabulum are usually not treated for 5 to 10 days post-obit the injury. Considering the patient experiences significant bleeding with this fracture, the orthopedic surgeon must await for the patient'southward own clotting mechanisms to get into upshot – usually within three to five days. During this menstruation the patient may be in traction to prevent additional injury.
Preoperative procedures
Patients scheduled for surgery undergo a number of tests. These include:
- Claret tests
- An electrocardiogram (or EKG) that tests the electrical activity of the heart
- A chest X-ray to ensure that the lungs accept not been injured and have no fluid in them and that the patient has no infection of the lung (pneumonia)
- Conventional radiographs (X-rays), computerized tomography (CT browse), or magnetic resonance imaging (MRI): Each of these tests helps the surgeon get every bit much information as possible near the fracture before offset surgery. CT scans are peculiarly useful since they allow the medico to see the fracture in several planes and too see a 3D model of the fracture on a computer monitor
- Magnetic resonance venogram (MRV): Assesses the patient's veins. Many patients with fractures of the pelvis and acetabulum develop claret clots in the veins of the pelvis, thighs or lower legs. If the clot travels through the body to the lungs it is called a pulmonary embolism and can interfere with the patient's breathing. If the MRV shows that a clot is present, treatment for the clot is immediately started. This may include placement of an Inferior Vena Cava Filter, that is a "strainer" in the major vein to the centre to prevent any blood clots going to the lungs (pulmonary embolism).
At HSS all surgery patients with fractures of the pelvis and acetabulum are given pocket-size preoperative doses of heparin (an anticoagulant), a drug that prevents clotting. Patients continue to have an anticoagulant (coumadin) later surgery until the dr. has ruled out any further danger of clotting.
In addition to these tests, doctors and nurses oft cheque the patient's pulses, the feeling in the injured limb, and ask almost any strange sensations such equally tingling or numbness in the limbs.
Postoperative care
Following surgery, managing the patient's pain and managing any complications that arise due to the injury are primary concerns.
Initially, pain medication will be given by injection. However, many patients are able to use a pump that controls the amount of pain medication given. This is known equally patient-controlled analgesia (PCA) and offers patients the benefits of managing his or her hurting. Since there is a maximum dose that can be delivered at whatever given time, there is no danger that the patient will receive also much medication.
Other medications that may be given include anticoagulants to thin the blood and avoid the development of blood clots, and Indocin, which prevents bone germination in areas around the muscles. (See "Complications" for more on why these drugs are given.)
Patients are encouraged to become upwards and out of bed as soon as possible, since doing so helps to avoid some of the complications associated with these injuries. A regimen of physical therapy is followed to maintain muscle force and range of motion during recovery.
After surgery to repair a pelvic fracture or fracture of the acetabulum, many patients continue to feel the effects of damage to nerves that might have occurred during the traumatic result or the surgery. Of import branches of the lumbar and sacral nerves may exist either stretched or torn, especially in the example of unstable pelvic fractures. Injuries to the nerves event in decreased feeling in a limb and/or difficulty or inability in moving part of the limb. It is hard to predict whether these nerves volition fully recover. Even so, the majority of patients practice regain some awareness and function of the limb inside 6 to xviii months after their injury.
What are the complications of surgery for a broken pelvis?
Throughout treatment and recovery, doctors and nurses are watchful for the following potential complications:
- Deep vein thrombosis and pulmonary embolism: Blood clots that may form in the veins of the pelvis, thighs, and/or lower legs and may travel to the lungs.
- Pneumonia: An infection of the lungs that may bear on any patient who is confined to bed and cannot expand his or her lungs equally fully as they ordinarily do.
- Skin Issues resulting from existence in one position for a long menses of fourth dimension
- Muscle Complications due to inactivity.
- Heterotopic Ossification, a condition in which the body mistakenly forms os in an area where in that location is usually musculus; prompt treatment is required to prevent this new bone from interfering with joint movement.
- Harm to the Head of the Femur: if the articular cartilage lining of the articulation is affected in an injury to the pelvis, and especially in fractures of the acetabulum, information technology's important to keep the surfaces of the joint from rubbing together-and to avoid the adventure of future development of arthritis. Preoperatively, traction or a system of ropes, pulleys and weights are used to relieve pressure in the joint. Apparently, surgery with open reduction and internal fixation is performed to realign the joint with plenty stability to let firsthand mobilization and hence preserve the polish lining of cartilage and avoid subsequent arthritis.
- Avascular Necrosis of the Caput of the Femur: Patients with a dislocated hip and/or fracture of the acetabulum may have disrupted blood flow to the caput of the femur (the ball in the hip joint). This tin result in death and plummet of os tissue and hip joint arthritis.
- Nutritional Bug: The body requires more protein and calories during healing.
- Constipation resulting from inactivity.
- Infection at the site of the injury
Patients who take suffered a traumatic accident or injury may experience psychological distress over changes in their advent and physical functioning. The stupor of becoming an accident victim may also linger. As with a serious disease, the patient may wonder "why me" and be searching for reasons the blow occurred. Difficulty sleeping and coping with the hurting associated with recovery are not uncommon. Patients with pre-traumatic depression or who are experiencing other stressful life events are more than prone to experience psychological difficulty connected with their fracture.
In many cases, the passage of fourth dimension eases these symptoms. At HSS patients and their families have telephone admission to trauma nurses with extensive feel in this field. Often they are able to address the questions and concerns that arise. When necessary, the patient's physician may recommend contact with a social worker or psychologist.
Outcomes
The outcome of surgery for a pelvic or acetabular fracture is dependent on a variety of factors including: the extent of injury including injuries to the head and other organs, the health of the patient prior to the injury, and whether this is the patient'southward outset surgery for the condition.
Pelvic fractures and the multiple injuries that often go along with them are potentially life-threatening. In improver, unfortunately, even those patients who survive these injuries and whose basic are successfully realigned and healed, may have a significant degree of long-term inability, and chronic hurting is not uncommon. Many accept injury to the genitourinary organisation that can result in incontinence and impotence. The best chance for a expert recovery lies in receiving excellent care from specialists who are experienced in rapid decision-making following a traumatic accident.
By itself, a fracture of the acetabulum is more often than not not a life-threatening injury. (Of course, some patients with these fractures will also have other serious injures.) And, thanks to advances in treatment over the years, especially surgical reduction and stabilization techniques, fourscore% to 85% of patients, tin can look a adept to first-class recovery post-obit surgery, provided that the hip can be properly aligned and fixed.
On the second mean solar day post-obit surgery for an acetabular fracture, patients are unremarkably able to get out of bed. Crutches must be used for eight weeks following surgery, but by 12 weeks most people are able to walk unassisted. If they are otherwise in practiced status, nearly people recover fully within four to six months and are able to resume recreational activities at that time.
For individuals who accept received initial treatment for their pelvic and acetabular fractures elsewhere, who have not healed properly, and are now seeking corrective surgery, a complete recovery can be more difficult to achieve. Merely previous surgery is not necessarily an obstruction to a good result following a second surgery, but this requires an experienced team, as this is the almost complicated and difficult surgery of all.
While many of us have become accustomed to the amazing strides achieved by medical scientific discipline, it's worth noting that these proficient results following acetabular fractures are remarkable. This progress is due in large office to long-term studies conducted by two French researchers, Judet and Letournel, who identified the common fracture problems and provided key information on the best style to gain access to the fracture with the to the lowest degree amount of injury to the patient. Based on their findings, amend instruments and surgical techniques have evolved. Physicians also take a better understanding of how to avoid complications and of the healing procedure. More recently, boosted data nigh the fracture is achieved through visualizing techniques such every bit CT and MRI scans. Before any of these developments occurred, patients with acetabular fractures had a far less promising outlook. Most concluded with painful arthritic hips, and in young patients a hip bone fusion, which resulted in drastically limited mobility.
The Orthopedic Trauma Service at HSS
The Orthopedic Trauma Service at HSS is a team of physicians, nurses, technicians, nutritionists and therapists who have been assembled to provide the best intendance possible to those people who have had a major musculoskeletal injury. We specialize in patients with circuitous injuries including fractures of the pelvis, acetabulum, other major joints (elbow, shoulder, hip, knee and ankle), calcaneus and long bone injuries.
Many of the patients treated for these fractures at HSS are referred by physicians at other institutions, or at the request of a family member. This process starts with a phone conversation between Dr. David Fifty. Helfet, the Managing director of the Orthopedic Trauma Service and the outside dr. who is currently treating the patient. Subsequently the patient's demand for treatment at HSS has been established, the trauma nurse at HSS speaks to the nurse currently in charge of the patient's care to obtain a head-to-toe assessment of the patient'due south condition. This information is relayed to the HSS/NYPH staff, in order to determine what other injuries are nowadays, whether the patient must first be transferred to the ICU and evaluated by the General Surgery Trauma Team (NYPH) or whether they are cleared and ready for surgery right away. In most cases, patients are not transferred until they are stabilized at the outside establishment and are able to undergo surgery the twenty-four hours post-obit their arrival at HSS/NYPH.
In some cases, information technology may be necessary to filibuster transfer until information technology has been adamant that the patient is stable for transfer and there is no ongoing injury present. Failing to exercise this could upshot in serious and permanent disability. While this waiting menstruum can be difficult for patients and their families, this is a precaution that must exist observed for the patient'southward safety.
Staff members from each hospital coordinate the condom transfer of the patient, which may be done by motorcar, ambulance, plane or helicopter depending on private circumstances. Owing to the staff and the infirmary's reputation for excellence, trauma patients have been transferred to HSS/NYPH from all over the globe for treatment of these fractures.
Frequently asked questions and answers
Q: Why practice I need surgery for a cleaved pelvis?
If your surgeon recommends surgery it is because y'all take a displaced fracture and there is an incongruity in the acetabulum. Normally the acetabulum is a polish cup, congruent with the femoral caput, allowing for frictionless movement of the femoral head. If the fracture heals in the displaced position and there is a "step off" then the cartilage on the femoral head volition wear abroad causing posttraumatic arthritis. This is painful and can be very debilitating and possibly may pb to a hip fusion or total hip replacement. The goal of the surgery is to:
- restore the normal shape of the acetabulum
- subtract hurting and allow for early ambulatory function
- decrease the hazard of mail-traumatic arthritis
- delay or avert the necessity for a total hip replacement
Q: How long will I exist in Hospital for Special Surgery?
The typical inpatient stay for acetabular fracture surgery is 7 to 10 days.
Q: Volition I have a brace or cast later surgery?
No. The fracture is reduced and stabilized internally with plates and screws.

Weight begetting will exist express for eight weeks following the surgery to permit the os to heal.
Q: Will I have a limp after the surgery?
Near patients that undergo aggressive rehabilitation to restore muscle forcefulness and flexibility do not have an abnormal gait but tin can walk normally.
Q: When exercise my sutures or staples come out?
10 to fourteen days later on surgery the patient returns to the surgeon for a post-operative check-up. At this time, the wound is examined and the sutures or staples are removed. The patient may shower or bathe later they are removed.
Q: Do I have to get to a rehabilitation facility after my stay at Hospital for Special Surgery?
No. Most of our patients do return home after their surgery. Concrete therapy in the hospital insures that each patient is independent on a walker or crutches and is able to manage stairs. However, at that place are certain situations where a patient prefers to get to a rehabilitation facility postal service-operatively and this can be worked out in the infirmary with the trauma social worker.
Q: When can I return to piece of work?
Typically patients with these injuries who do manual labor are on temporary disability for six to ix months following surgery. Those individuals that have jobs that are less physically enervating, ie. desk jobs, render to work much earlier (some fifty-fifty after a few weeks). However, each case is evaluated on an individual footing.
Q: How much pain will I be in afterwards surgery?
Pain is very subjective, nonetheless, at HSS a complaint of pain is taken very seriously and every effort is made to adequately command the pain. Well-nigh patients exercise get home with oral medication.
Q: How long do I need to become to physical therapy?
Strengthening and flexibility exercises are very of import components of the rehabilitative process. Most of the exercises necessary to increment strength such every bit running on the treadmill and or using the stationary wheel do not commence until total weight bearing at eight weeks. Most patients will continue with concrete therapy for half dozen to 12 months later surgery.
Q: How long will I exist under the care of my surgeon?
Initially y'all volition see your surgeon every couple of weeks and have conventional radiographs. At almost 6 months you will return approximately every 3 months for X-rays followed by annual check-ups. Additional visits are unnecessary unless a trouble arises.
Q: Is there whatsoever medication I can accept or anything I can practise to expedite the healing procedure?
No. A fractured bone typically takes eight weeks to heal. There is no medication to speed upwardly the healing. A healthy diet and adequate sleep are ever recommended. Of notation, smoking has been known to delay healing and sometimes arrest healing all together.
Q: My family member was brought to the infirmary today with a fracture of the acetabulum, just we were told that surgery to repair the broken bone won't take place for at least a week even though she doesn't have other injuries. Shouldn't she be treated right away?
This delay will actually protect your relative. An acetabular fracture is accompanied past a significant amount of haemorrhage. Over the class of the adjacent three to five days bleeding will terminate with the assistance of the body'due south own clotting mechanisms. Merely after this happens is information technology safe to proceed with surgery.
Q: I will be undergoing repeat surgery for a pelvic fracture that happened three years ago. What are my chances for improved function and practiced recovery?
Unfortunately, in that location's no precise answer to this question. The success of the surgery depends on the potential for improving the alignment of the broken bones, your overall health, and power to adhere to a rehabilitative program. While it is always easier to get expert results with an initial repair of a fracture, previous surgery does not necessarily hateful that you will not experience significant comeback.
Q: Why is information technology sometimes necessary to have more than one operation to fix a pelvic fracture? Tin't the surgeon fix everything at one time?
In many cases, the surgeon must approach the pelvic bones from dissimilar directions in club to consummate the repair. Each of these approaches tin can crave a separate surgery.
Q: I understand that I will have to start taking a blood thinning drug earlier undergoing surgery for an acetabular fracture. Will that put me at greater risk for excessive bleeding?
Your md has prescribed this medication for you to guard against the development of a blood jell in the veins of your pelvis, thighs or lower legs. Should such a clot develop and travel to your lungs, information technology can interfere with breathing and pose a meaning danger. You will be taking a very low dose of this medication and will be watched carefully to ensure that no excess bleeding occurs.
Q: My grandmother broke her acetabulum after a simple autumn in her home. How could this happen?
Your grandmother probably has osteoporosis, a condition in which the bone density decreases and the bones become more than fragile and likely to break on impact. If she has non been assessed for this status before, her physician will certainly do and then and recommend a course of handling to help prevent future fractures.
Updated: 12/17/2019
Summary Prepared by Nancy Novick • Diagnostic imaging examinations provided by HSS Radiologists
Authors
Source: https://www.hss.edu/conditions_pelvic-fractures-acetabular-fractures.asp
Posted by: morrislosenaloo.blogspot.com



0 Response to "How To Repair A Fracture"
Post a Comment